It has been shown that pregnancy can cause sclerosis at the SIJs in the postpartum period (≥ 2 years after childbirth), whereas pregnancy-/birth-related BME along the SIJ seems to vanish after the first postpartum year.
This study by Christoph Germann published in Skeletal Radiology adresses important open question questions:
Do SpA-related subchondral sclerosis differs from pregnancy subchondral sclerosis?
Does the birth method (vaginal delivery or cesarean surgery) impact the subchondral sclerosis?
Are number of children have an impact on the extent of sclerosis?
https://link.springer.com/article/10.1007%2Fs00256-020-03700-9
The data shows that
- Pregnancy has no impact on long-term BME on SIJ.
- Pregnancy may cause long-term subchondral sclerosis—similar to SpA-associated sclerosis.
- Number of children is positively correlated with SIJ sclerosis.
- Birth method yields no effect on SIJ sclerosis.

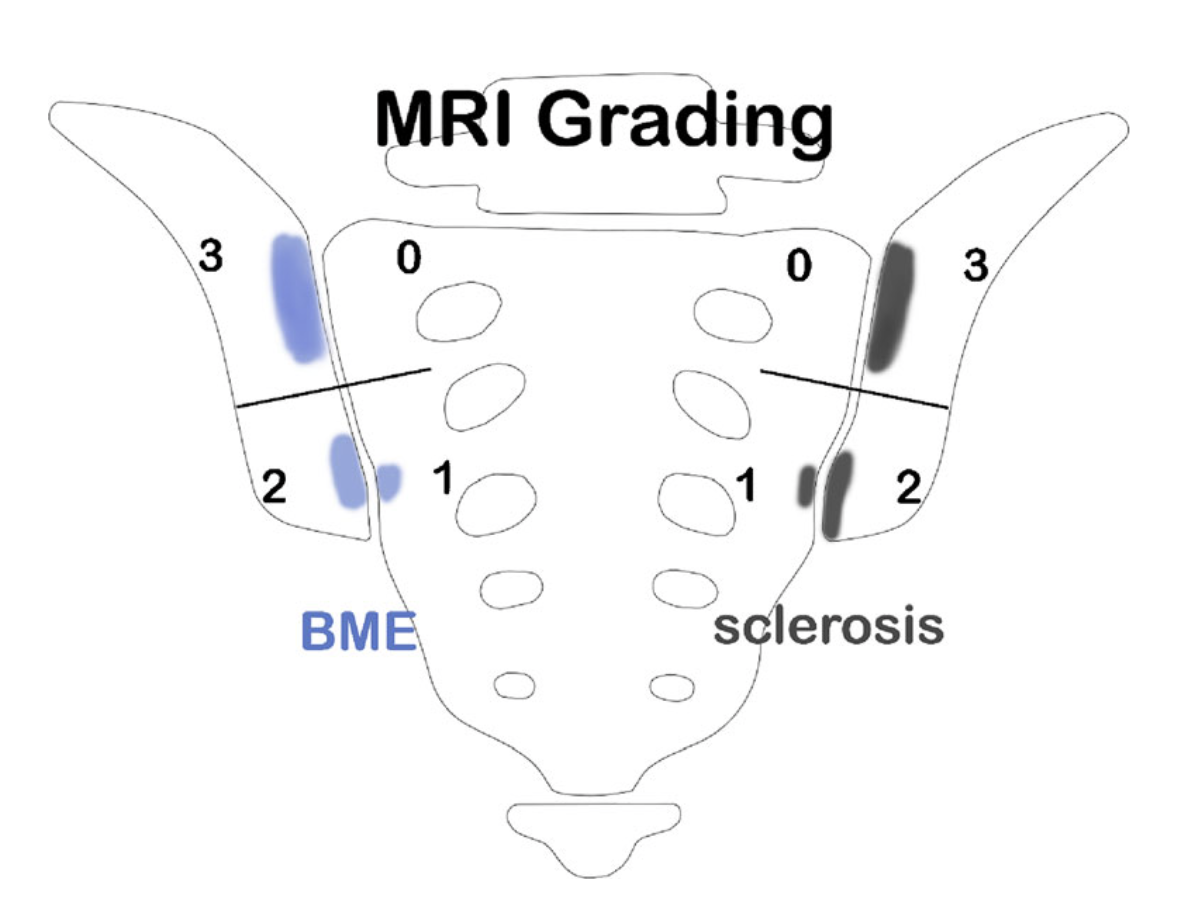
Oblique coronal view on SIJ with illustration of quadrant-based grading system (Berlin method). Both SIJ are divided into 4 quadrants, respectively, each of which is graded separately in a semiquantitative manner in regard to presence of BME and sclerosis: not present (score = 0), < 33% of quadrant area (score = 1), ≥ 33 to <66% of quadrant area (score = 2), and ≥ 66% of quadrant area (score = 3). Right SIJ depicts BME score 0 to 3, left SIJ depicts sclerosis score 0 to 3, respectively. BME bone marrow edema, SIJ sacroiliac joint
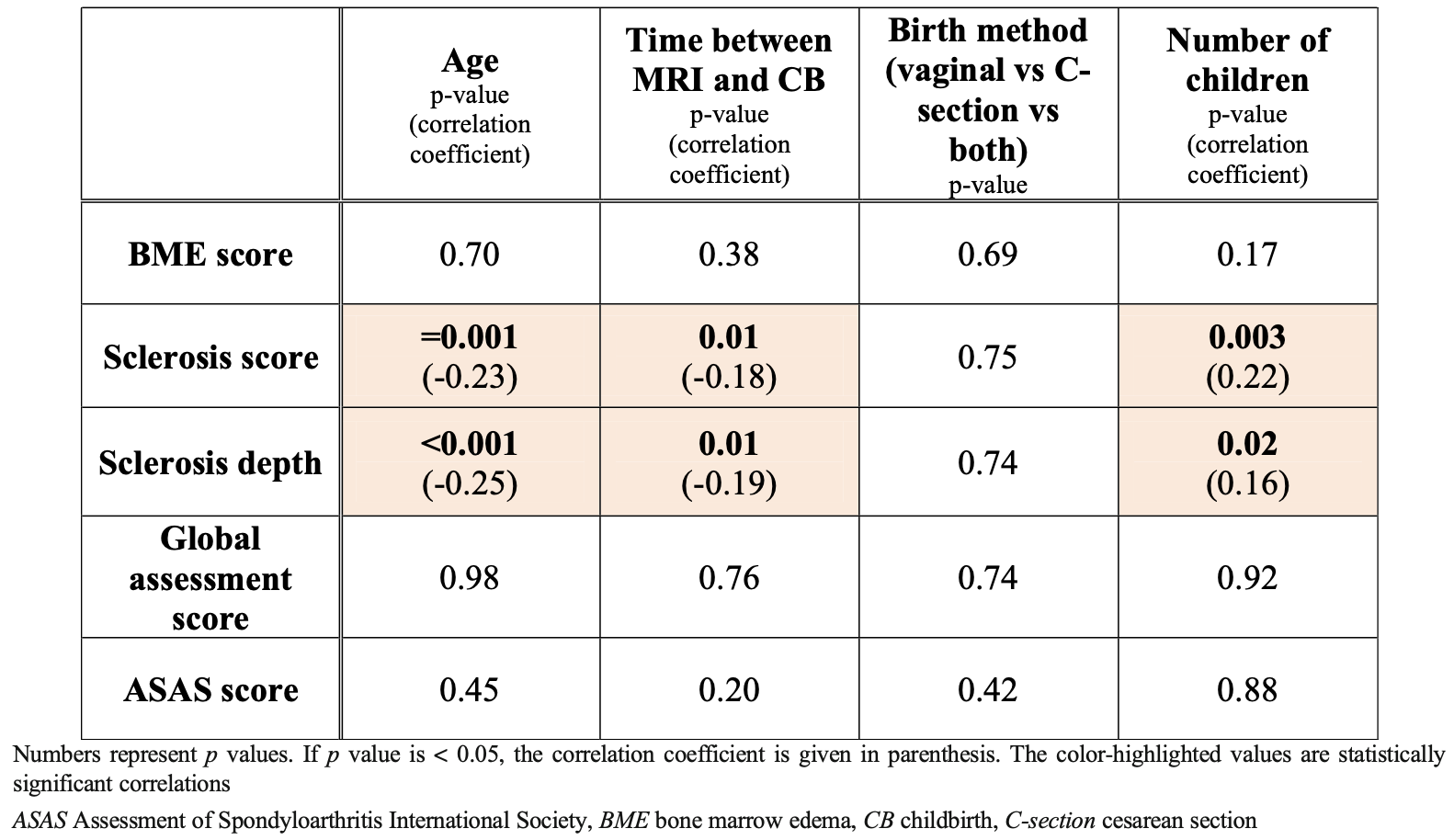
Correlation analysis in the SpA negative subgroup after pregnancy: Table illustrates the influence of age and childbirth-related factors on BME, sclerosis, overall assessment score, and ASAS score.
